Resources
How Healthcare Transparency Data Enabled Fair Reimbursement in Anthem-Covenant Negotiations
For months, a dark cloud of uncertain negotiations between Covenant Health and Anthem loomed over 14,000 patients, fostering fear that their providers would be cut from the Anthem network. According to a spokesperson for Anthem, negotiations stalled because “Covenant Health continue[d] to insist on double-digit rate increases that are more than three times the rate of inflation and, as a result, refused our offers to keep care affordable.”
Covenant Health’s spokesperson countered that their goal was “to structure an agreement that provides fair reimbursement for our providers and hospitals and continues to offer our patients access to the medical services they need at an affordable rate.”
On July 5th, the day the existing contract was set to expire, the negotiators fortunately reached a favorable conclusion to “provide Mainers with the highest quality care and best patient experience possible,” according to the recent press release.
Why negotiations between Covenant and Anthem nearly failed, and how data enables fair reimbursement rates from payers.
An essential aspect of the healthcare system is the interaction between medical providers and health insurance companies. As a private medical provider, Covenant depends on reimbursement from healthcare plans for the wide range of procedures they perform. In contrast, companies like Anthem, a payer in this equation, negotiate the extent to which they cover the cost of specific medical procedures.
In these negotiations, knowledge is power. Until the Transparency in Coverage rule of 2022 mandated payers to make their rates public, healthcare providers like Covenant operated in the dark, lacking crucial information needed to negotiate fair reimbursement rates. Prior to the Transparency in Coverage rule, if Anthem told Covenant Health that they were paid in line with other similar providers, Covenant would have had to take Anthem’s word for it. Providers like Covenant might suspect the data told a different story, but the absence of this data often forced them into a corner during payer negotiations.
Although the Transparency in Coverage rule now requires payers to release reimbursement rate data, it’s hardly user-friendly. These datasets are vast, machine-readable files, their size dwarfing even the entire Netflix HD catalog of movies. Interpreting this data requires formidable computational resources and teams of expert developers. Here’s where a tool like Pulse medical tool by HexIQ can enter the equation and turn the tide for healthcare providers.
Pulse turns massive, cryptic files into a trove of invaluable insights, shedding light on the reimbursement landscape.
When HexIQ learned of the ongoing negotiations between Covenant Health and Anthem, the team utilized the Pulse medical tool to reveal that there was much more to Anthem’s assertion that Covenant demanded unfair increases to existing reimbursement rates. In fact, the data revealed that Covenant was operating at a severe disadvantage. For a hospital that services 14,000 patients, reimbursement rates often sit at a median value between the highest and lowest rates offered by a payer, but Covenant reimbursement rates for the most commonly used procedures were at or near the lowest in the state.
Rates for spinal fusions, joint replacements, and uterine procedures were the lowest in the state of Maine. Not only that, other codes with significant gaps between the lowest and highest reimbursements were reimbursed at the lowest end of the spectrum at Covenant Hospitals.
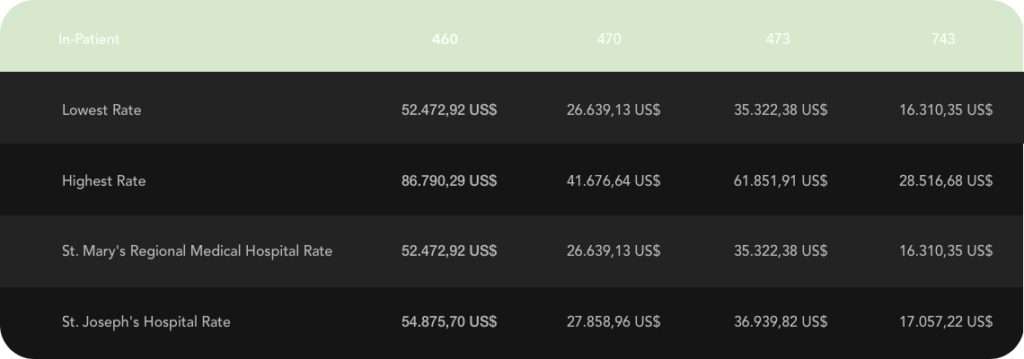
For example, code 19120, “Ablation, Exploration, and Excision” has a reimbursement range of $237.26 and $2,365.35. Covenant was reimbursed at a mere $279.13, significantly lower than the median value. Similarly, for the code 11602 – “Excision of Malignant Lesion”, Covenant’s reimbursement rate of $114.46 was only a few dollars more than the lowest rate in Maine of $110.06, a figure far removed from the highest rate of $932.61. This trend of disproportionately low reimbursement rates persisted across numerous procedure codes, with reimbursements consistently between 36% and 43% lower than the highest negotiated rate in the state.
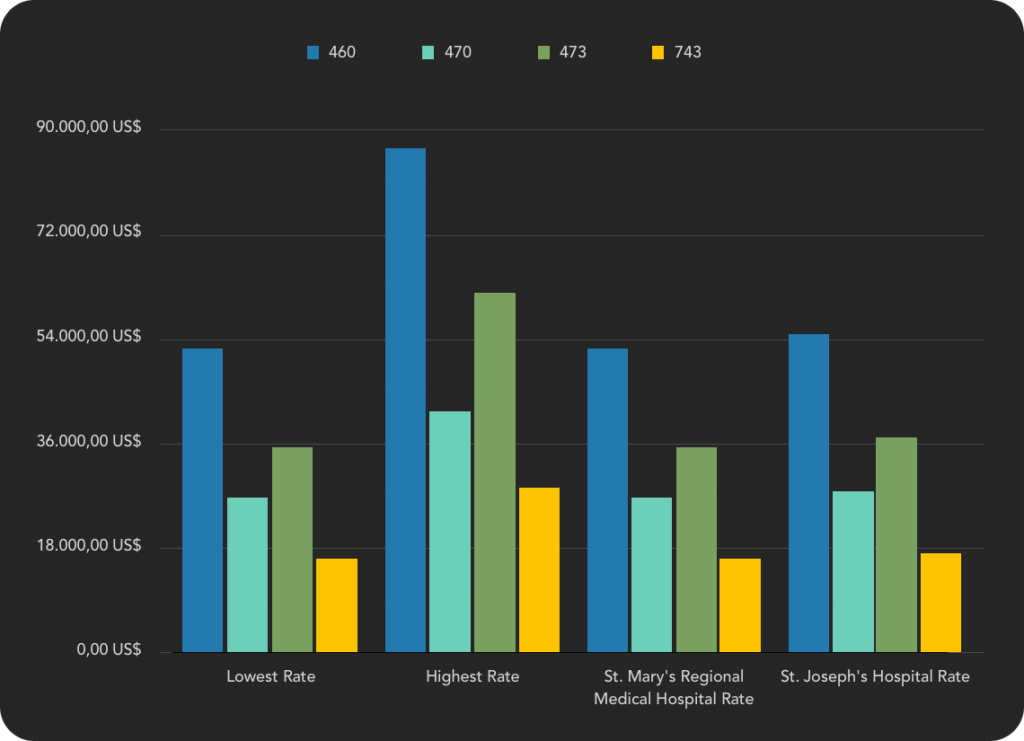
The data supports Covenant’s position; doubling existing reimbursement rates is not an unreasonable demand that exceeds 3x the rate of inflation, but rather represents a fair rate that places them in the median range of rates where they belong for the number of providers, procedures, and patients serviced.
Once obscure, rate reimbursement data is now an invaluable tool that enables providers to effectively counter payer resistance to fair negotiations. This data, provided by tools like Pulse, tells a story that empowers a fair market price for healthcare providers. Through informed persistence, providers like Covenant can ultimately negotiate successful agreements that reflect a more equitable reimbursement structure.
Through data-driven insights, providers can demonstrate a resolute commitment to their patients and staff and ensure fair pricing for their services.
This story illuminates the potential of data science tools like Pulse, which can empower any healthcare provider to negotiate from a position of strength.